What are thyroid tumors?
Thyroid lumps
Types of thyroid nodules (information on each disease is provided in a separate section)
“Thyroid lumps” are scientifically referred to as “thyroid nodules.” Thyroid nodules are either tumors or tumor-like lesions. Tumors are classified as benign or malignant. Tumor-like lesions are defined as “hyperplasia.” They are benign, resulting from a proliferation of cells that are the same as functional tissue. Malignant tumors must be followed closely. The goal of examinations and testing is to determine whether a tumor is benign or malignant.
Nodules can be generally divided into the following five types (according to General Rules for the Description of Thyroid Cancer):
- 1. Benign tumors
- 2. Malignant tumors
- 3. Other tumors
- 4. Unclassifiable tumors
- 5. Tumor-like lesions
Benign tumors are follicular adenoma, and types of malignant tumors include papillary carcinoma, follicular carcinoma, poorly differentiated carcinoma, medullary carcinoma, undifferentiated carcinoma, and malignant lymphoma. Most tumor-like lesions are benign. They include adenomatous goiter and cysts.
Examinations and testing
In general, a characteristic feature of thyroid tumors is for patients to have lumps but report no other symptoms. Patients undergo examinations to determine whether a tumor is benign or malignant (cancer).
Visual inspection and palpation
Visual inspection and palpation of the neck area where the thyroid is located are performed to determine the presence and size of lumps and assess their attributes (hardness, extent, etc.)Blood tests
These tests measure levels of thyroid hormones and thyroglobulin (Tg), a protein synthesized in thyroid tissue, in the bloodstream.Ultrasonography (echography) of the neck region
An ultrasound device (probe) is placed around the neck to emit ultrasonic waves. The reflected waves or “echoes” are converted into images to use for diagnosis. In addition to examining a lump’s size, shape, and location, this technique is used to judge whether malignancy can be suspected.Echo-guided fine-needle aspiration biopsy cytology (aspiration biopsy cytology)
A fine needle is inserted into thyroid lumps to collect cells, which are subsequently examined under a microscope. The needle used in the test is as thin as those for taking blood.Computed tomography (CT scan) examination
An image of the body’s interior is made using X-rays. This technique is primarily employed to investigate whether cancer has metastasized or spread to surrounding organs. Fine-grained images of inside the body are successively taken from various angles to obtain detailed information.Isotope test
For this test, radioactive iodine is administered to the patient. The tiny amount of radiation emitted by the iodine in the body is captured and converted into images by a special device called a gamma camera. This examination not only reveals the size and shape of thyroid lumps, but also assesses thyroid function and determines whether recurrence or metastasis of cancer has occurred. The examinations listed above do not always diagnose the type of nodule. In such cases, patients may undergo surgery (requiring hospitalization) to receive a more accurate diagnosis. The tumor is removed and examined in detail under a microscope (histopathological examination).Benign tumors
The condition of an enlarged thyroid gland is generally called “goiter.” For the case when there is swelling in a part of the thyroid in the form of a lump, the term “nodular goiter” is used. Nodular goiter can be benign or malignant. Benign nodules include follicular adenoma, adenomatous goiter, and thyroid cysts. Whereas follicular adenoma is a true tumor, adenomatous goiter occurs when thyroid cells proliferate (known as “hyperplasia”) and develop in the shape of a lump. Adenomatous goiter and adenomatous nodules are observed more often than follicular adenoma.
Types
◆Follicular adenomaThe size of this type of nodule goiter varies from barely palpable to very large such that a patient cannot look down.
◆ Thyroid cysts Only a small proportion of thyroid cysts actually meet the definition of a “true cyst.” Most thyroid cysts are actually secondary cysts, either adenomatous goiter or follicular adenoma that have internally degenerated or undergone bleeding that causes swelling like a water balloon. However, there is no difference in clinical approach, and both types are diagnosed as cysts.
Malignant tumors
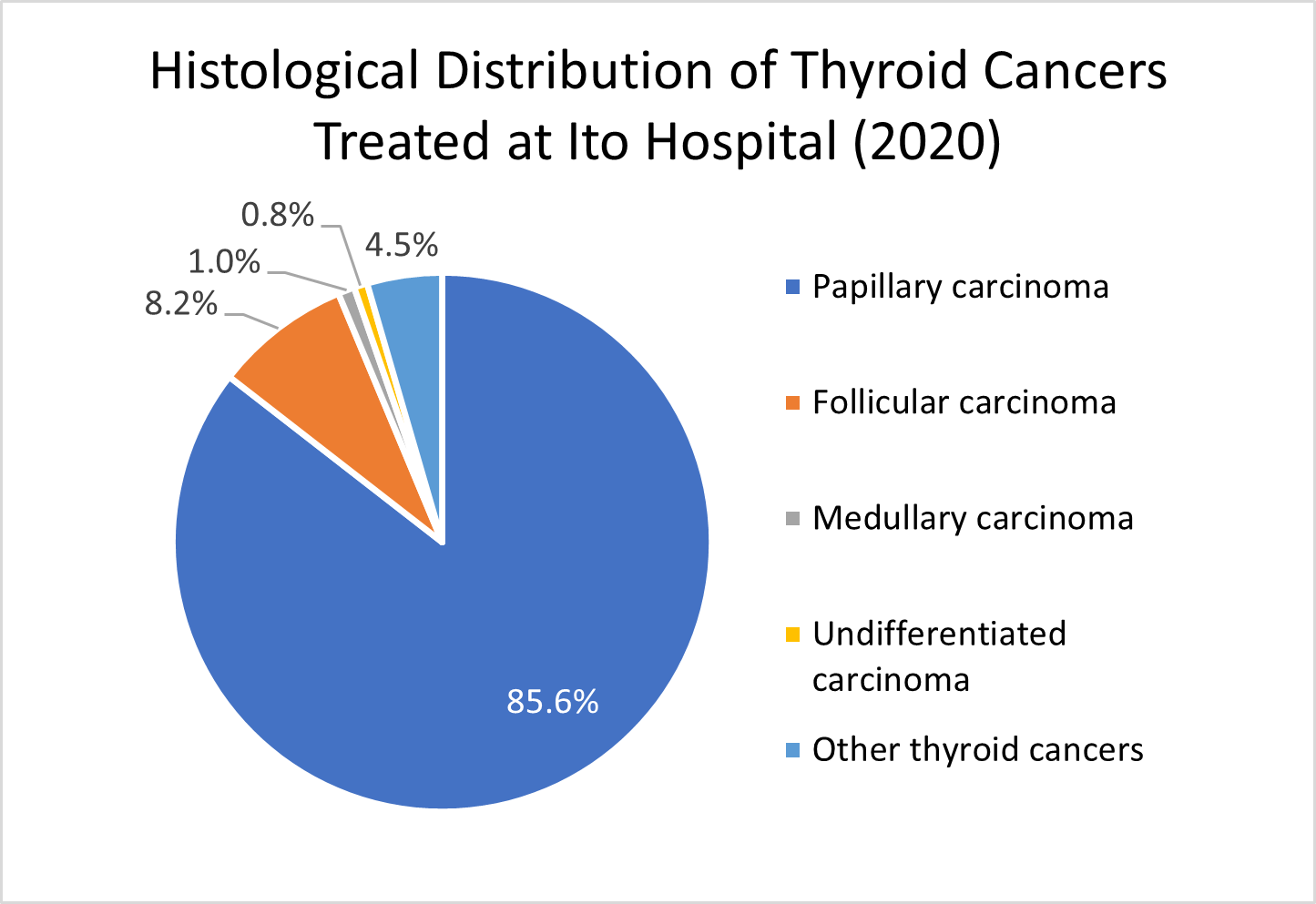
Most thyroid lumps are “benign” and only a very small proportion are “cancer.” Thyroid cancer accounts for approximately 1% of all cancers. The incidence of thyroid cancer is three times higher in women than men (according to national cancer incidence data). Compared to other types of cancer, thyroid cancers progress slowly and most can be cured. Thyroid cancers include papillary carcinoma, follicular carcinoma, poorly differentiated carcinoma, medullary carcinoma, and undifferentiated carcinoma. According to aggregate statistics reported by the Japanese Society of Thyroid Surgery, the relative proportions of the cancer types are papillary carcinoma (92.5%), follicular carcinoma (4.8%), undifferentiated carcinoma (1.4%), and medullary carcinoma (1.3%). The chart below shows the distribution of cancer types treated at Ito Hospital in 2020. Papillary carcinoma and follicular carcinoma are also termed “differentiated carcinomas” since their cells are mature, and their growth is slow.
The human body consists of cells. Cells with more complex and specialized functions are said to be more differentiated (mature). Consequently, cancer cells that have a high level of differentiation do not easily metastasize. In contrast, cancer cells with low differentiation tend to metastasize comparatively easily.
(1) Papillary carcinoma Accounting for more than 90% of thyroid cancer is “papillary carcinoma.” A docile form of cancer, papillary carcinoma progresses slowly. In general, there are no symptoms other than lumps. However, when the lumps start to get large, people may experience a variety of symptoms, including discomfort, pain, difficulties swallowing, and a hoarse or husky voice. In recent years, an increasing discovery rate of cancer stems from the use of ultrasonography on the neck region during regular medical check-ups. When lumps are detected, people seek care at hospitals. Papillary carcinoma seldom metastasizes in distant organs. However, it is not uncommon for papillary carcinoma to spread to the lymph nodes around the thyroid during relatively early stages. Therefore, some people notice an abnormal swelling of the lymph nodes on the side of the neck. However, a distinctive feature is that even if papillary carcinoma metastasizes in the lymph nodes, it still develops slowly and treatment at this stage often leads to full recovery. For patients who have undergone surgery at Ito Hospital, the 20-year survival rate is higher than 90%. Papillary carcinoma is an extremely curable form of cancer.
(2) Follicular carcinoma Follicular carcinoma accounts for approximately 5% of thyroid cancer. Similar to papillary carcinoma, the presence of lumps is the only abnormality in most cases. While this type of cancer rarely invades the lymph nodes, it may metastasize in distant locations, such as the lungs and bones. However, follicular carcinoma progresses slowly. If treated early, the rate of recovery is quite high. For patients treated at Ito Hospital, the 10-year survival rate is 89.9%.
(3) Poorly differentiated carcinoma Some types of papillary carcinomas and follicular carcinomas have components with low levels of differentiation on the histological level. These cancers are called poorly differentiated carcinomas. Since poorly differentiated carcinomas progress a littlet faster than common papillary and follicular carcinomas, they have a somewhat higher degree of malignancy and require appropriate treatment.
(4) Medullary carcinoma Medullary carcinoma is a unique form of cancer, accounting for approximately 1-2% of all thyroid cancer cases. Unlike papillary carcinoma and follicular carcinoma, which develop from follicular cells that produce thyroid hormones, medullary carcinoma develops from parafollicular cells (C cells). Parafollicular cells produce calcitonin, a hormone that lowers calcium levels in the blood. Approximately 2/3 of medullary carcinomas arise by chance (sporadic) and 1/3 are hereditary in nature. For the hereditary type, approximately half of blood relatives have the potential of developing the same kind of cancer (autosomal dominant inheritance). Hereditary medullary carcinomas are associated with diseases in other endocrine glands, such as pheochromocytoma (adrenal tumors) and hyperparathyroidism, in a condition known as multiple endocrine neoplasia (MEN). Genetic testing has made it possible to detect the presence of genes that cause hereditary medullary carcinoma.
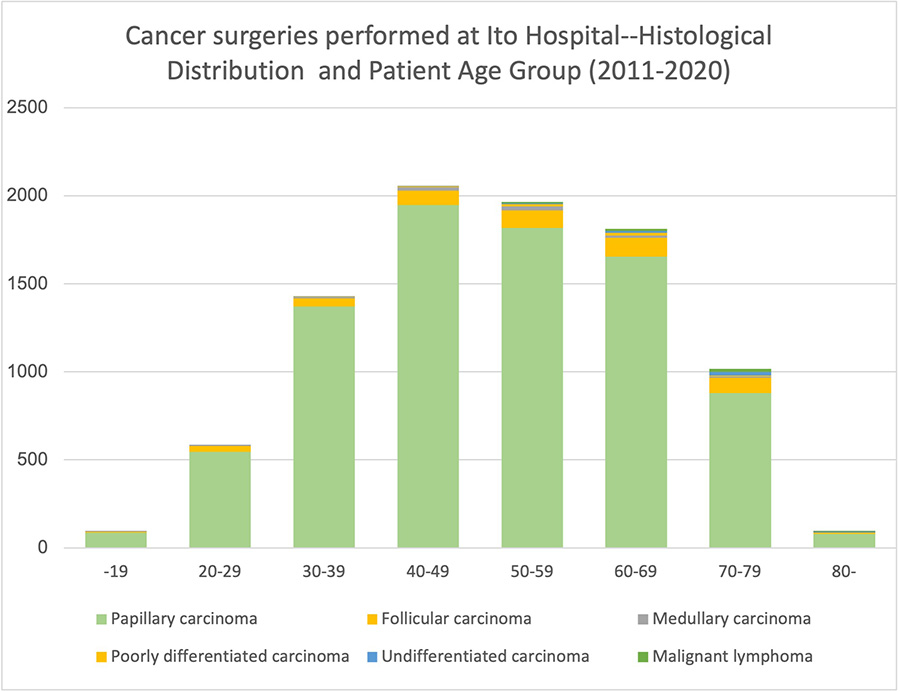
(5) Undifferentiated carcinoma Since undifferentiated carcinoma cells are extremely immature, this type of carcinoma progresses rapidly and is highly malignant. Undifferentiated carcinoma occurs most commonly in the elderly, has a male-to-female ratio of 1:2, and accounts for approximately 1-2% of thyroid cancer cases. The figure below shows the age distribution of thyroid cancers treated at Ito Hospital. Thyroid cancer is found in people of all ages, from youths to the elderly. While papillary carcinoma and follicular carcinoma occur most commonly in people in their 40s-60s, undifferentiated carcinoma predominately afflicts people aged 60 and older. In general, cancers in young people tend to progress rapidly and are difficult to treat. However, thyroid cancer is an exception. Since thyroid cancer is highly treatable, please undergo medical examinations as soon as possible after noticing a lump. There are other varieties of malignant thyroid tumors. One type is malignant lymphoma, which occurs rarely. For information regarding malignant lymphoma, please follow this link.
Treatment
After diagnosing lumps as benign or malignant, appropriate treatment and management methods are considered.Treatment of benign nodules
If lumps are benign tumors, in most cases they will not interfere with daily life even when left untreated. However, if a patient is concerned about large or conspicuous lumps, treatment may be considered. Options include percutaneous ethanol injection therapy (PEIT) and surgery. Also, in the case that the possibility of cancer cannot be excluded, surgery is also considered.(1) Percutaneous ethanol injection therapy (PEIT) In this treatment method, a type of alcohol (ethanol) is injected, causing a nodule to shrink. This therapy has two effects. First, a direct injection into a nodule causes necrosis. Second, an injection into the blood vessels suppresses the delivery of nutrients to a tumor. Recently, this therapy is commonly used for “thyroid cysts.”
(2) Surgery Thyroid nodules can enlarge and cause intense pressure on the trachea or spread and descend into the area behind the clavicle (mediastinum). In these cases, we recommend surgery to remove the nodules.
◇“Partial thyroidectomy” to “total thyroidectomy” This treatment method removes lumps that have formed in the thyroid. While the approach depends on the lump’s attributes, the standard practice is to remove the lump and the side of the thyroid where it is located. In addition, when performing this type of surgery, another aim is to leave parathyroids, located at the back of the thyroid, in the body. In the case that parathyroids are removed with the thyroid, we transplant the tissue inside the body (muscle) in order to avoid hypoparathyroidism after surgery.
Treatment of malignant tumors
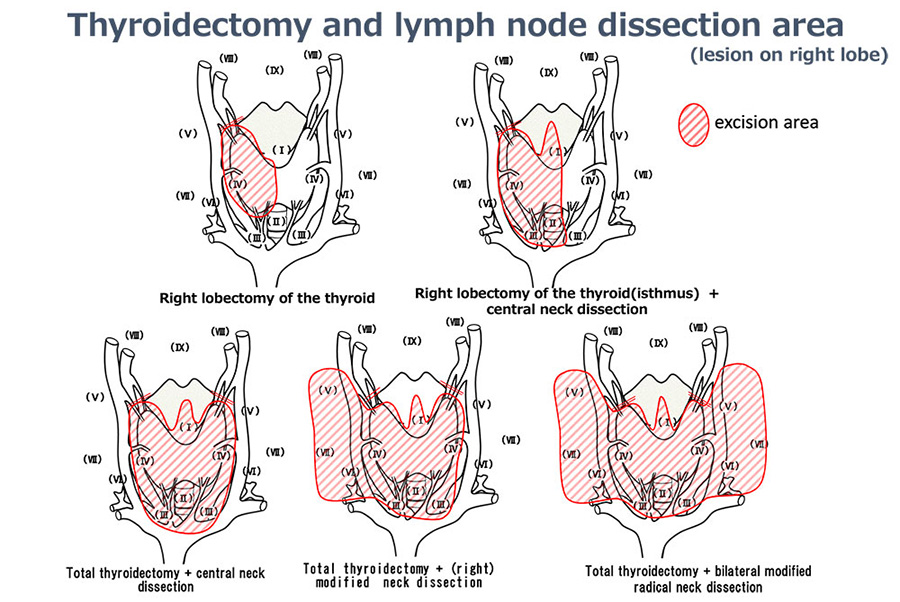
For thyroid cancer, surgery is the basic treatment. Since thyroid cancer progresses slowly, the cancer can usually be removed, including metastases in the lymph nodes.(1) Surgery The areas of thyroid excision and lymph node dissection is determined according to the degree of a cancer’s progression.
◇Thyroidectomy area: “partial thyroidectomy” to “total thyroidectomy” ◇Lymph node dissection area: “central neck dissection” to “bilateral modified radical neck dissection”The area of thyroid removal and lymph node dissection varies according to the spread of the disease (number and size of lesions; location of swollen lymph nodes). Similar to surgery for Basedow’s disease and benign tumors, parathyroids are in principle left in place or transplanted to muscles in the neck.
(2) Isotope therapy (radioactive iodine oral medication) Thyroid cells absorb iodine that has been consumed in meals. The cells use the iodine as raw material to make thyroid hormones that are secreted into the bloodstream. In the same fashion as iodine ingested during meals, radioactive iodine is also absorbed by the thyroid. While in the thyroid gland, radioactive iodine emits radiation that reduces the number of thyroid cells. Thyroid cancer cells that have metastasized also absorb radioactive iodine. As a result, radioactive iodine is taken in by metastasized thyroid cancer where it destroys the cancer cells from the inside. Surgery is the primary treatment for malignant tumors. However, in the case that cancer cells have metastasized in the lungs or other distant organs, isotope therapy is used after the entire thyroid has been removed. Radioactive iodine is used in thyroid function examinations and treatment for Basedow’s disease. However, for cancer treatment the amount ingested is extremely small. Basedow’s disease treatment, for example, uses several dozen times the amount of radioactive iodine. Since this therapy uses radioactive iodine, special equipment and facilities are required. Only a limited number of institutions are suitably equipped. Ito Hospital has been providing isotope therapy since 1955.
◇ Isotope ablation When total thyroidectomy is performed to treat thyroid cancer, a small amount of thyroid tissue called the “thyroid bed” is left in the area between the trachea and where the thyroid gland was located. It has been shown that the destruction (ablation) of this residual portion of the thyroid gland using radioactive iodine reduces future recurrence of cancer. This method is standard in Europe and the USA. Ablation is performed in patients with lymph node metastasis or cancerous invasion of surrounding organs. (In should be noted that this technique is not performed for all patients who undergo a total thyroidectomy.) In Japan, ablation was originally approved only for inpatient treatment. However, guidelines have changed and now it is possible to perform ablation therapy on an outpatient basis provided certain conditions are fulfilled. Ito Hospital has been performing outpatient ablation therapy since September 2011. Thus, both inpatient and outpatient ablation therapy have become possible. In preparation for therapy, patients follow an iodine-restricted diet for two weeks. Patients also need to discontinue thyroid hormone medication for approximately 4 weeks before therapy and may experience symptoms of hypothyroidism (lethargy, drowsiness, cold sensitivity, etc.) in the time surrounding therapy. In 2012, however, it became possible to continue hormone therapy using a therapeutic injection (Thyrogen*). (Payment for the injection and an additional two days of examination is required.)
*What is Thyrogen? Thyrogen is a drug that acts in the same fashion as thyroid-stimulating hormone (TSH), which promotes the production of thyroid hormones. In isotope testing and therapy, it is important to stimulate the thyroid to incorporate a large amount of radioactive iodine in order to improve the diagnostic accuracy of the examination or increase the therapy’s effects. For this purpose, two types of preparation are required: restriction of iodine intake and elevation of blood TSH levels. Previously, discontinuation of thyroid hormone medication before an examination or treatment was the only way of increasing TSH levels. However, in recent years health insurance has covered the drug Thyrogen, a new method of increasing TSH levels. Since this method does not require discontinuation of thyroid hormone medication, patients can undergo isotope tests and treatment without having to endure the various symptoms of hypothyroidism. However, both methods have advantages and disadvantages. We encourage patients to select a course of therapy according to the conditions of their disease.
(3) External beam radiotherapy (linear accelerator [LINAC]) In this type of therapy, cancerous lesions are irradiated with high-energy X-rays. This can shrink or destroy tumors. The device used to emit the X-rays is a LINAC (linear accelerator). Since Ito Hospital does not have the necessary facilities, we will issue request to another institution if a patient needs this form of treatment.
(4) Molecular targeted therapy The primary treatment of thyroid cancer is surgery. After surgery, however, relapse may occur. If the cancer reappears in a location where surgery is impossible or it is accompanied by distant metastases, patients will undergo either oral radioactive iodine therapy or TSH suppression therapy. Yet, these treatments may be ineffective. In such cases, molecular targeted therapy is pursued. It uses a recently developed and approved class of drugs that attacks the molecular mechanisms of the appearance and spread of thyroid cancer. Specifically, the medications are tyrosine kinase inhibitors (sorafenib, Lenvatinib, and vandetanib) that suppress tumor growth and aim to more effectively treat the disease.
Effects Cancer cells encourage the growth of new feeder blood vessels to obtain nutrients. Molecular targeted drugs primarily inhibit the growth of these blood vessels, thereby exerting antitumor effects (shrinking tumors).
Suitable medications (insurance approved items) The type of medication that can be used depends on the variety of thyroid cancer.
| Medication | Use |
|---|---|
| Sorafenib | Papillary carcinoma, follicular carcinoma, medullary carcinoma |
| Lenvatinib | All types of thyroid cancers |
| Vandetanib | Only medullary carcinoma |
| Medication | Main side effects |
|---|---|
| Sorafenib | Hand and foot syndrome, high blood pressure, diarrhea, etc. |
| Lenvatinib | High blood pressure, diarrhea, proteinuria, low appetite, thrombocytopenia, etc. |
| Vandetanib | Rash, diarrhea, clouding of the cornea, electrocardiographic abnormalities, etc. |
Starting treatment At Ito Hospital, patients are admitted for an approximately one-week stay when starting oral medication for molecular targeted therapy. Side effects are monitored, and patients receive guidance about necessary precautions and the management of medications. Thereafter, treatment is conducted on an outpatient basis. (5) TSH suppression therapy After surgery, thyroid hormone medication is administered to prevent recurrence. Secretion of thyroid hormones is promoted by thyroid stimulating hormone (TSH), which is secreted by the pituitary gland at the base of the brain. Conversely, if thyroid hormone levels increase too much, the secretion of TSH is suppressed. TSH promotes the proliferation of both benign and malignant tumor cells. This mechanism is basis for treatment using thyroid hormone medication. By administering a somewhat higher amount of thyroid hormone, this kind of treatment aims to suppress the secretion of TSH, thereby preventing the proliferation of tumor cells. The effect reduces the possibility of recurrence. TSH suppression therapy is not carried out after all thyroid cancer surgeries. It is recommended for patients who have a high risk for recurrence or metastasis.