- What is Basedow’s disease
- Symptoms
- Symptoms associated with Basedow’s disease (not connected to thyroid function)
- Examinations and testing
- Treatment
- Daily Life
- Pregnancy and Basedow’s disease
What is Basedow’s disease?
Basedow’s disease is a typical disorder that causes hyperthyroidism, a condition in which thyroid hormones are overproduced. Since thyroid hormones are an important factor in stimulating metabolism, overproduction can lead to burdens on organs throughout the body. As a result, Basedow’s disease is associated with a variety of symptoms.
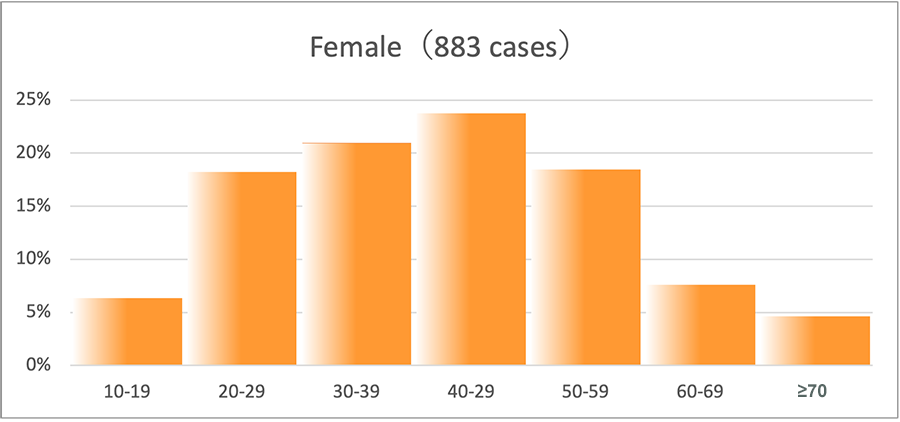
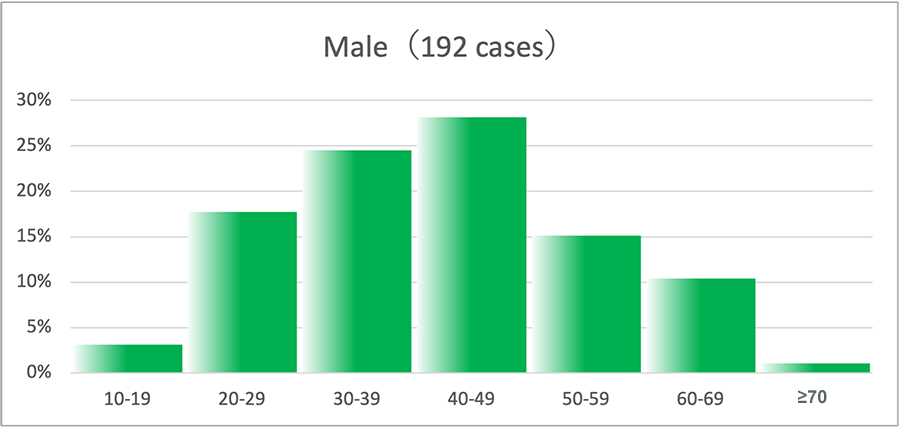
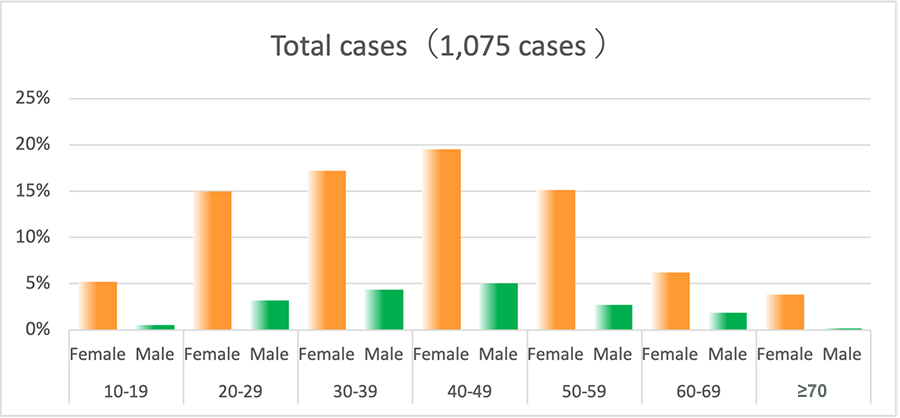
Gender and age distribution
Basedow’s disease is common in women. For every man with Basedow’s disease, there are approximately 5-6 women who suffer from it. It tends to occur in people in their 20s to 50s, and most commonly in those in their 20s to 40s.
Age distribution of patients with Basedow’s disease at the time of their first visit to Ito Hospital (new, untreated patients in 2020)
Basedow’s disease is common in women. For every man with Basedow’s disease, there are approximately 5-6 women who suffer from it. It tends to occur in people in their 20s to 50s, and most commonly in those in their 20s to 40s.
 Disease name origin
Disease name origin- Basedow’s disease was named after the German physician Karl Adolph von Basedow who published research on this disease in 1840. Since Japan draws from the German medical tradition, the disease is referred to as Basedow’s disease in Japan. In the United States and some other European countries, the disorder is known as “Graves’ disease,” named after the Irish doctor Robert James Graves.
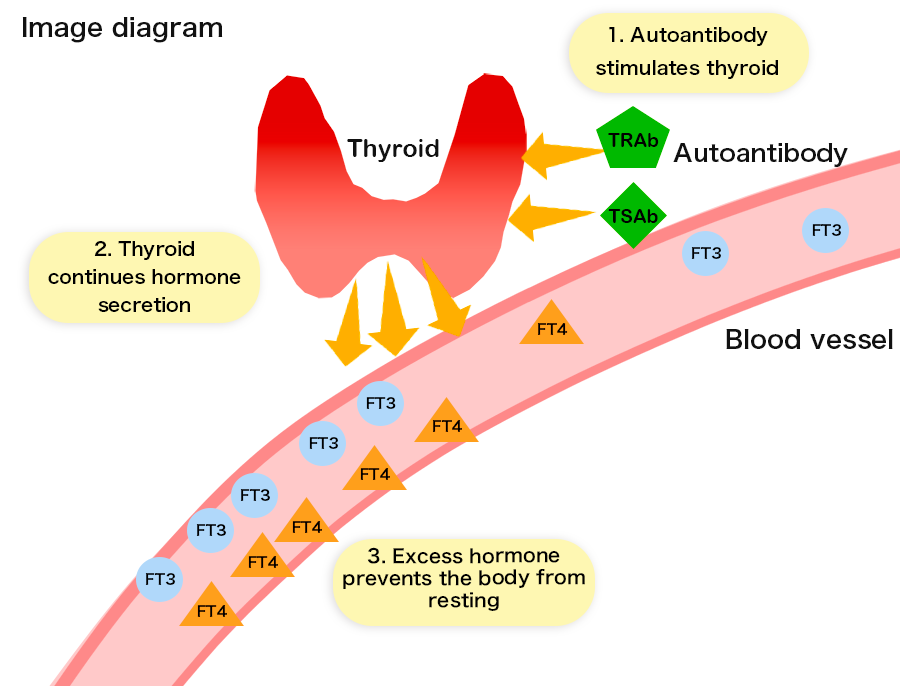
Basedow’s disease and “autoimmunity”
Development of Basedow’s disease is related to abnormalities in the immune system. The immune system plays an important role in protecting the body by producing “antibodies” that fight against external enemies such as viruses and bacteria. However, if the body produces antibodies that attack itself (autoantibodies) rather than external intruders, then it can cause disease. This is termed an “autoimmune disorder,” and Basedow’s disease is an example. It is still not clear why this kind of antibody is produced. In Basedow’s disease, autoantibodies (TSH receptor antibodies: TRAb and TSAb) stimulate the thyroid gland to overproduce thyroid hormones.
Causes of Basedow’s disease
Multiple causes are thought to be involved in the development of Basedow’s disease. Presently, no definitive cause has been identified. It is believed that genetic and environmental elements are involved. Regarding the environment, potential external factors are injury and stress, and internal factors include pregnancy and childbirth.
Symptoms
Basedow’s disease has three symptoms (the Merseburg triad) that have long been well-known. When Basedow’s disease was first discovered, these symptoms (listed below) were described as characteristic of the disease. Since advances in testing have made early detection possible, a variety of other symptoms have also been identified.(1) Goiter (swollen thyroid gland)
(2) Bulging eyes (thyroid-associated ophthalmopathy)
(3) Tachycardia (rapid heartbeat)
Goiter
“Diffuse goiter,” a condition in which the entire thyroid gland swells, is present in most cases of Basedow’s disease. However, some patients may have differences in the swelling on the right and left sides of the thyroid. There are also patients whose swelling is barely detectable.
■ Normal thyroid gland
■ Diffuse goiter
Symptoms due to overproduction of thyroid hormones
Thyroid hormones stimulate the body’s metabolism. When there is an excess of thyroid hormones, metabolism increases to an abnormal level and the entire body continues to work energetically without rest. As a result, a variety of symptoms can occur, including excessive sweating, sensitivity to heat, increased appetite, and weight loss.
In addition, internal organs work vigorously. Since the heart is easily affected, symptoms such as palpitations, rapid heartbeat, arrythmia, and heart failure can occur. Intestinal peristalsis also becomes energetic, leading to irregularities in bowel movements (loose stool, diarrhea, frequent bowel movements). Other common symptoms include tremors in hands and feet, muscle weakness, and fatigue. Since emotional instability, insomnia, and poor concentration are also known to occur, adults may see drops in efficiency at work and children’s academic achievement may decline. Blood tests detect changes due to increased metabolism. These include increases in glucose levels as well as decreases in cholesterol, lipids, and other fats. Bone metabolism, in which old bone is absorbed and new bone is created, also increases speed. However, it has been demonstrated that the production of new bone is insufficient. Bone density decreases and the risk of osteoporosis elevates for post-menopausal women and the elderly.
These symptoms originate from the overproduction of thyroid hormones, and they improve after hormone levels are returned to normal. However, arrythmia and heart failure may linger. In these cases, it is necessary for patients to also receive care from a cardiologist. In addition, since smoking hinders the effectiveness of treatment for Basedow’s disease, it is of the utmost importance that patients do not smoke.
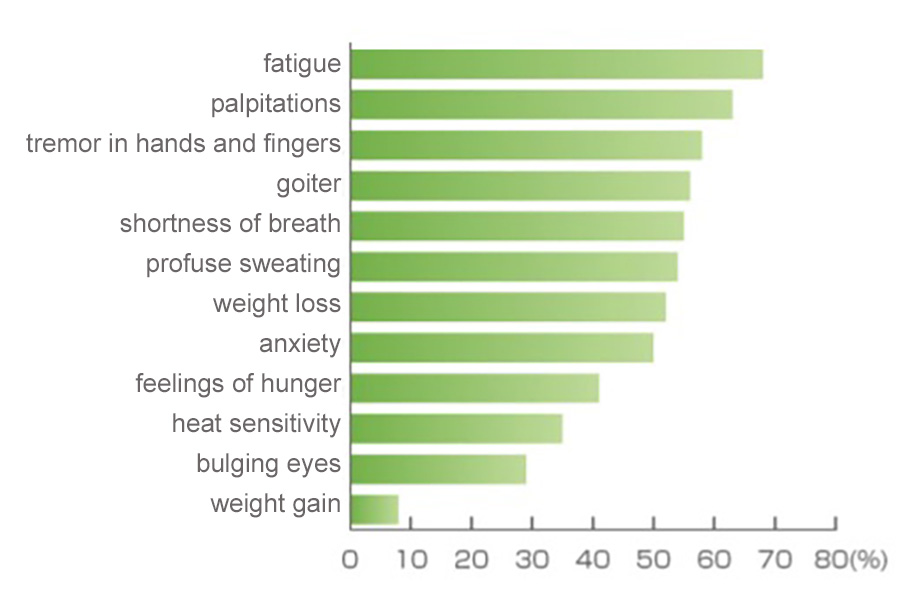
Figure 1 shows symptoms present in pretreatment Basedow’s disease patients who received care at Ito Hospital in order of frequency.
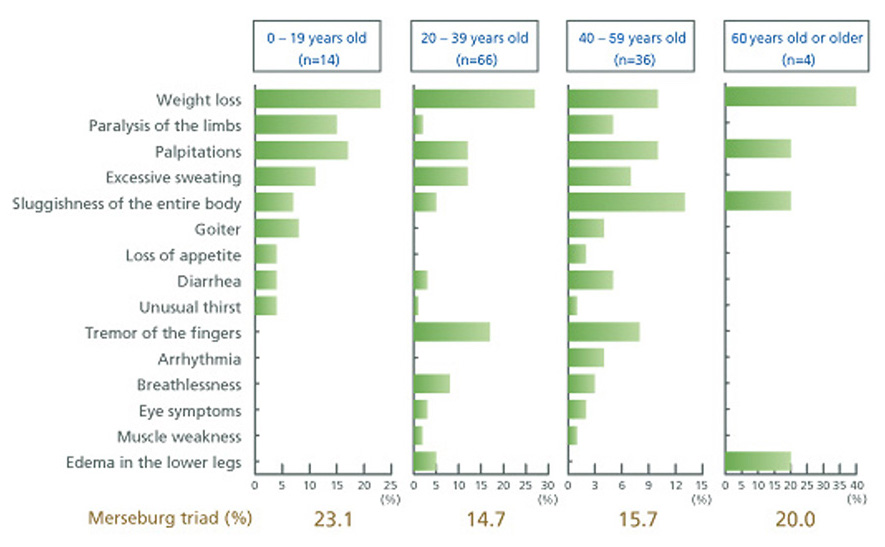
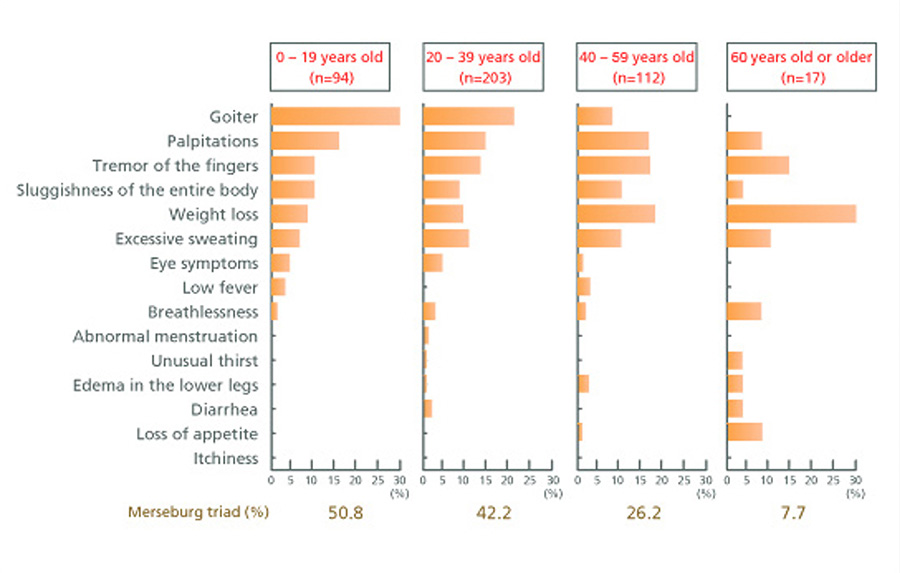
Variation in symptoms in relation to age group
Basedow’s disease has a variety of symptoms with large individual differences in their expression. As shown in Figures 2-1 and 2-2, age groups also show different patterns of symptoms. Thyroid swelling stands out in young patients but is rare in elderly patients. On the other hand, weight loss is common in elderly patients, while many young patients have increased appetite and weight gain.
Special Pathologies due to overproduction of thyroid hormones
Thyroid stormPatients who do not receive sufficient treatment can suffer thyroid storm. This condition occurs when an individual encounters severe stress, such as injury, infection, or surgery for non-thyroid related problems. Multiple organ failure is a result. The condition may arise early in treatment or due to taking oral medication at irregular times. Also, cessation of medications for the purpose of examinations may trigger thyroid storm. Symptoms include delirium, fever (>38℃), rapid heart rate (>130 beats per minute), diarrhea and other intestinal problems, jaundice, and heart failure. Although treatment methods are advancing presently, the condition is still life threatening. It is important to receive proper treatment and maintain stable thyroid function.
Thyrotoxic periodic paralysisPeople who have hyperthyroidism may not be able to move their limbs the next morning following strenuous exercise or bouts of overeating and overdrinking (especially carbohydrates or alcohol). This is a result of a rapid decline in the mineral potassium (K) in the bloodstream. It has been reported that the condition is common for Asian males.
Symptoms associated with Basedow’s disease
(not connected to thyroid function)
Thyroid-associated ophthalmopathy
Beginning with bulging eyes, eye symptoms (thyroid-associated ophthalmopathy) have long been well-known and are characteristic of Basedow’s disease. At the time of diagnosis of hyperthyroidism, patients often display thyroid-associated ophthalmopathy. However, some patients develop eye symptoms after treatment begins, while others exhibit eye symptoms before developing hyperthyroidism. Since improvement of thyroid function alone does not resolve eye symptoms, it is necessary for patients to see an ophthalmology specialist for testing and treatment.
(1) Bulging eyes Behind each eye, there is adipose tissue and muscles that move the eye. If they enlarge due to inflammation or edema, the eyes are pushed forward, causing bulging eyes. If the protrusion is severe, patients may experience reddening of the eye’s surface membrane (conjunctiva) and corneal ulcerations. These conditions can be painful.
(2) Lid retraction Lid retraction occurs when the muscles that raise the upper eyelids experience tension or inflammation, thereby preventing the eyelids from descending. When thyroid hormone levels are high, the eyelids may retract due to muscle tension. This type of lid retraction can be remedied by taking antithyroid medications that return hormone levels to their normal range. However, when lid retraction is caused by inflammation, direct treatment of the ophthalmopathy is required.
(3) Diplopia (double vision) Inflammation of the muscles that move the eyes causes them to swell, worsening eye movement. As a result, the left eye and the right eye do move in alignment, and people will see two images of a single object. This condition is called “diplopia” (double vision). It is known that these eye symptoms are exacerbated by smoking. While treatment from an ophthalmology specialist can be expected to alleviate symptoms, smoking cessation is critically important.
Pretibial myxedema
Pretibial myxedema is a condition in which a portion of the skin on the tops of the feet and around the ankles swells and darkens. There are reports that steroid treatments ameliorate this condition, but the effectiveness varies from individual to individual.
Examinations and testing
Blood tests and in some cases isotope tests (radioactive iodine with thyroid scintigraphy) are used to diagnose Basedow’s disease. Also, ultrasonography is used to assess thyroid size and detect the presence of nodules (lumps). Since high levels of thyroid hormones place a burden on the heart, chest radiography and electrocardiography are used when there is a suspicion of heart problems, such as arrhythmia or heart failure.
(1) Blood tests A blood test is carried out in order to detect abnormalities, including elevated thyroid hormone (FT3 and FT4) levels, low thyroid-stimulating hormone (TSH) levels, and high TSH receptor antibody (TRAb, TSAb) levels.
(2) Radioactive iodine (isotope) uptake test (scintigraphy) This test evaluates the status of thyroid function. In the case that blood test results for TRAb and TSAb are negative, this examination is used to avoid complete reliance on diagnosis through blood tests. The properties of radioactive iodine result in its incorporation (absorption) into the thyroid. If thyroid hormone production is excessive, as in the case of Basedow’s disease, the incorporation rate will be high. There is also a form scintigraphy that uses technetium rather than radioactive iodine.
Precautions regarding isotopeTo undergo testing that uses radioactive iodine, it is necessary limit intake of food containing iodine for seven days before the examination. Since a radioactive substance is used, pregnant women cannot undergo this examination. In addition, women who are breastfeeding must cease breastfeeding for three days, including the day of the examination. A detailed explanation will be given when a test is performed.
(3) Ultrasonography This examination is performed to assess the size of the thyroid and detect the presence of tumors.
(4) Electrocardiography This examination measures heart rate and detects the presence of arrhythmia and other heart disorders.
(5) Chest radiography This examination measures the size of the heart and determines whether there is a shadow on the lungs.
Treatment
There are three main methods of treatments: oral medication (antithyroid drugs), isotope (radioactive iodine) therapy, and surgery. In most cases, treatment starts with oral medication, and then other treatments are considered in relation to the progress in the patient’s condition, the presence of tumors, eye symptoms, and other factors.
1. Treatment with medication
This method is based on regular ingestion of medication that inhibits the synthesis of thyroid hormones. Medications include antithyroid drugs and inorganic iodine.Antithyroid medicationsThere are two types of antithyroid medication, thiamazole (Mercazole®) and propylthiouracil (Thiuragyl®/Propacil®). These medications will not result in immediate changes, but effects will appear 2-3 weeks after beginning a regimen. Hormone levels generally fall to a normal range after 2-3 months. However, side effects occur most easily in the period of 2-3 months after starting medication. During this time, it necessary to visit the hospital every two weeks. A suitable dosage is administered based on a patient’s condition. Taking medication consistently and without interruption allows thyroid hormone levels to be maintained in a normal range. If medication is abruptly halted because thyroid hormone levels decline, a swift relapse occurs. It is vital to continue taking medication in accordance with a prescription. Treatment with oral medication is usually necessary for at least two years. There are also cases when medication is required for a significantly longer period of time. Cessation of drug treatment is considered when more than six months have passed with a patient maintaining normal thyroid function while taking a daily dosage of antithyroid medication of one tablet or less per day and, at that point, TSAb and TSAb levels are also normal. In the year following the conclusion of drug-based treatment, changes in thyroid hormone levels are common. As a result, it is necessary to monitor thyroid function once every 2-4 months. Unfortunately, if medication is the only form of treatment, few patients experience remission (a stable condition without medication). If Basedow’s disease recurs, treatment will need to be restarted. If there is a pattern of repeated recurrence, then we recommend the primary treatment methods of surgery or isotope therapy.
【Side effects of antithyroid medication】 The side effects listed below may occur while taking antithyroid medication. It is important to understand the issues and regularly visit the hospital for examinations.
(1) Itchiness and rash These side effects occur in approximately 5% of patients, usually appearing 2-3 weeks after beginning drug-based treatment. For light cases, anti-allergic medication can be taken with antithyroid medication, allowing for the treatment regimen to continue. If the addition of anti-allergy medication fails to result in improvements or there is a worsening of symptoms, it will be necessary to cease antithyroid medication.
(2) Liver dysfunction Liver dysfunction occurs most often in the period of 2 weeks to 3 months following the start of antithyroid drug treatment. A blood test is needed to provide confirmation each time. Liver function may also fluctuate due to changes thyroid hormone levels. As a result, it is important to determine whether changes in liver function are due to the influence of antithyroid medication or shifts in hormones. At Ito Hospital, we have observed liver dysfunction sufficient to consider cessation of antithyroid medication in 2.5% of patients. The portion who suffered particularly severe problems was 0.2%. Regarding the type of medication, it is thought that liver dysfunction occurs more frequently with propylthiouracil (Thiuragyl® / Propacil®) than thiamazole (Mercazole®). In most cases, cessation of antithyroid medication alone leads to improvement of liver function. However, some serious cases of liver dysfunction require hospitalization. Liver dysfunction is difficult for patients to notice, but if the skin and eyes (the white portions) take on a yellowish hue while taking antithyroid medication, it is necessary to halt the regimen and take a blood test to assess liver function.
(3) Agranulocytosis (granulocytopenia) This side effect occurs most often in the period of 2 weeks to 3 months following the start of antithyroid drug treatment. A blood test is needed to provide confirmation each time. Granulocytes are a type of white blood cell found in the blood. Agranulocytosis occurs when the number of granulocytes is severely reduced. Since granulocytes protect against viruses and bacteria that invade the body, individuals are unable to respond to such pathogens when suffering from agranulocytosis (granulocytopenia). While there are asymptomatic cases that are discovered through blood tests, agranulocytosis is commonly accompanied by a high fever and a severe sore throat. At Ito Hospital, the observed rate of agranulocytosis is 0.2%. However, the condition can be life threatening. If symptoms of agranulocytosis are observed while taking antithyroid medication, it is necessary to halt the regimen and take a blood test to assess the white blood cell (granulocyte) count. While agranulocytosis develops most often within the period of 2 weeks to 3 months after starting an antithyroid medication regimen, it may occur thereafter. It is necessary to remain vigilant.
(4) Other rare side effects: • Joint pain Pain mainly occurs in the joints of the arms and legs, but the location can shift.
• ANCA-associated vasculitis This condition primarily results from the medication propylthiouracil (Thiuragyl® / Propacil®). In some cases, only fever and joint pain occurs. In others, there may be vascular inflammation of the kidney or lung, which can cause renal or pulmonary damage. This side effect may occur several years after starting medication. If symptoms such as fever or joint pain occur while following the drug regimen, an examination will be performed.
Inorganic iodine medicationInorganic iodine is the raw material for thyroid hormones. However, if inorganic iodine is absorbed in excess, it can suppress the secretion of thyroid hormones for a period of time. This effect can be used to treat Basedow’s disease, though the duration of the therapeutic effect varies from individual to individual. For some people, the effectiveness dissipates after about two weeks. For others, inorganic iodine medication may remain effective for months or even years. At Ito Hospital, this treatment is frequently used in combination with antithyroid medication in the early stages of therapy. Inorganic iodine medication is also offered as a substitute drug to patients who are in a stage when they cannot take antithyroid medication due to side effects or other problems.
2. Isotope (radioactive iodine) therapy
Iodine is the raw material for thyroid hormones. After iodine is absorbed in the body, it is taken in by the thyroid gland where it is used to synthesize thyroid hormones. Isotope (radioactive iodine) therapy involves orally ingesting a radioactive isotope of iodine. The isotope is taken in by the thyroid gland where it destroys thyroid cells, thereby reducing the production of hormones. Although isotope therapy uses radiation, it does not lead to cancer, leukemia, immunosuppression, or other damage caused by radiation. Isotope therapy can be performed safely. If you are considering having children, contraception is necessary for 6 months for men and 1 year for women. Afterwards, there are no problems. After isotope therapy, thyroid-associated ophthalmopathy worsens in approximately 1% of patients. For this reason, it is necessary to be examined by an ophthalmology specialist beforehand to evaluate whether isotopy therapy is possible. In addition, patients should regularly have ophthalmological examinations to assess any changes in eye symptoms. In the days before and after therapy, it is necessary to limit iodine consumption. Also, regimens of antithyroid medication and inorganic iodine medication must be suspended. Because this therapy uses radiation, we do not in principle provide it to patients younger than 18 or to women who are pregnant or breastfeeding. Since this therapy uses radioactive iodine, special equipment and facilities are required. Institutions that are equipped for it are limited. Ito Hospital has been providing isotope therapy since 1955.
3. Surgical treatment
In this method, thyroid tissue that oversecretes thyroid hormones is surgically removed. This alleviates the condition of excess thyroid hormones. At Ito Hospital, when it is preferable for patients to receive surgical treatment, the standard surgical procedure is a “total thyroidectomy” in which no thyroid tissue is left in place. For this reason, patients need to start taking thyroid hormone medication after surgery. Thyroid hormone mediation (Thyradin-S®) has few side effects. It can be prescribed for long periods of time if dosages are stable, and the number of visits to the hospital decreases.【Advantages of total thyroidectomy over partial thyroidectomy】 (1) There is no recurrence of Basedow’s disease. (2) Levels of TSH receptor antibodies (TRAb) generally normalize earlier with total thyroidectomy than with partial thyroidectomy. For patients who hope for pregnancy soon, normalizing TRAb levels is a potential merit of total removal.
Selecting a therapeutic approach Each of the three therapeutic approaches has its own advantages and disadvantages. It is necessary to consider a patient’s condition, age, social situation, and other individual factors when selecting an appropriate method of treatment. In addition, since a patient’s condition may change during the course of treatment, the therapeutic strategy may be altered accordingly.
| Medication | Isotope (radioactive iodine) therapy | Surgery | |
|---|---|---|---|
| Appropriate patients | Patients of all age groups who meet the following conditions: ・ability to take medication regularly ・have small goiters *However, not all medications are suitable for small children and women who are pregnant or breastfeeding. Medications must be chosen appropriately. | Patients must not be pregnant, breastfeeding, or plan to be pregnant in the near future. In addition, patients must be at least 19 years old and meet one or more of the following conditions: ・Repeated relapses with medication ・Medication does not lead to improvement ・Experience side effects from medication ・A desire for a swift remedy | Patients who meet one or more of the following conditions: ・Difficulty healing with medication ・Experience side effects from medication ・Large goiters ・A desire for a swift remedy ・Thyroid tumors ・Eye symptoms |
| Advantages | ・Treatment can proceed on an outpatient basis. ・Treatment can start the day of diagnosis. | ・Therapeutic effects can be achieved in a shorter period of time than with medications. ・The incidences of complications and side effects are low. ・Relapse is not common. ・Therapy can be repeated. | ・Therapeutic effects can be achieved earlier than in other treatments. ・Antithyroid drugs can be discontinued the day after surgery. ・There is no recurrence. ・Thyroid hormone medication can be prescribed for long periods of time. |
| Disadvantages | ・Long periods of treatment are often necessary. ・Relapse is common. ・Side effects are possible. | ・A single therapy session may be insufficient. ・Cessation of antithyroid medication can take 1 year or longer. ・Patients may develop hypothyroidism. ・Hospitalization is necessary for elderly individuals as well as patients with a large goiter, heart problems, diabetes, or other complicating factors. ・Thyroid ophthalmopathy may worsen. | ・Scars remain. ・Patients develop hypothyroidism (thyroid hormone medication must be taken permanently). ・There is the possibility of complications from surgery. ・A hospital stay is required. |
Daily Life
Precautions for daily life
When thyroid hormone levels continue to be high, it places a burden on the heart that can easily lead to tachycardia and arrythmia. Please avoid vigorous exercise and activities that increase heart rate. If treatment returns thyroid function to a normal range, patients can lead a regular life, including exercise.Meals
There are no restrictions on diet. Patients are free to eat kelp and other kinds of seaweed that contain iodine as usual. When thyroid hormones are overproduced, metabolism and appetite increase together. When hormone levels begin to lower and metabolism returns to a normal range, appetite may not decrease as readily. During these times, it is easy for patients to gain weight. However, weight gain is not a side effect of antithyroid medication.Regular hospital visits
Regular hospital visits are an important part of treatment. When receiving drug-based therapies, any interruption of medication leads to instability of patient’s condition. Thyroid function may decrease after isotope therapy and surgery results in the patient needing thyroid hormone supplementation. In both cases, regular visits to the hospital are necessary. The gap between hospital visits varies according to a patient’s condition.Smoking
Smoking is not only harmful for eye symptoms, but it also decreases the effectiveness of treatment with antithyroid medication. We recommend smoking cessation and avoiding environments with tobacco.